Below are various excerpts from research studies and published articles by medical professionals, followed by full articles.
To gain an overview of the science for the arterial read this article-https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3394104/.

Breakthrough in Clinical Cardiology: In-Office Assessment with Pulse Wave Velocity (PWV) and Digital Pulse Analysis (DPA)by Brian Scott Peskin, BSEE, with Robert Jay Rowen, MD – 2010
“This article explores ‘an exciting, noninvasive, easy-to-use, and economical method of assessing patients’ cardiovascular physiologic status that is backed by more than 25 years of advanced research in medical physics”.
“Digital Pulse Analysis (DPA) is the next evolution in pulse wave velocity (PWV), and is based on the measurement of reflected infrared light (IR).”
“Numerous independent confirmations show statistically significant CV parameters based on age, and how PWV is the ideal method for assessing arterial stiffness and central aortic pressure.”
“Measurements are highly reproducible in clinical application and apply to both male and female patients.”
Better Management of Cardiovascular Diseases by Pulse Wave Velocity: Combining Clinical Practice with Clinical Research using Evidence-Based Medicine by Ali R. Khoshdel, MD, Shane L. Carney, MD, PhD, FRACP, Balakrishnan R. Nair, MD, PhD, FRACP, and Alastair Gillies, MD, PhD, FRACP.
“After reviewing 97 studies where PWV was measured, 5 end-stage renal disease patients, 5 hypertensives, 2 diabetics, and 2 elderly studies were selected. Pooling the data by the “fixed-effect model” demonstrated that the mortality and cardiovascular event risk ratio for one level increment in PWV was 2.41 (1.81–3.20) or 1.69 (1.35–2.11), respectively. There was a significant difference in PWV between survived and deceased groups, both in the low and high-risk populations. Furthermore, risk comparison demonstrated that 1 standard deviation increment in PWV is equivalent to 10 years of aging, or 1.5 to 2 times the risk of a 10 mmHg increase in systolic blood pressure. Evidence shows that PWV can be beneficially used in clinical practice for cardiovascular risk stratification. Furthermore, the above risk estimates could be incorporated into currently used cardiac risk scores to improve their predictive power and facilitate the clinical application of PWV”.
Arterial Stiffness and Cardiovascular Events: The Framingham Heart Study, by Gary F. Mitchell, MD, et al. (Circulation. 2010;121:505–511)
“In this study, we assessed the incremental value of adding pulse wave velocity [PWV] … to a risk model that includes standard risk factors for a first cardiovascular event. … Adding pulse wave velocity led to significant reclassification of risk and improvement in global risk prediction. … We need to focus our efforts on identifying and implementing interventions that can prevent or reverse abnormal aortic stiffness in order to prevent a marked increase in the burden of disease potentially attributable to aortic stiffness.”
The European Society of Hypertension (ESH) and the European Society of Cardiology (ESC) have added PWV measurement as an early index of large artery stiffening in their 2007 Guideline for the Management of Arterial Hypertension.
2007 Guidelines for the Management of Arterial Hypertension The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)
“Pulse-wave analysis at peripheral sites: Other techniques were derived from peripheral waveform shape analysis. The determination of the amplitude ratios of the second derivative of the pulse pressure waveform, obtained by finger photoplethysmography was used to study the effects of ageing and vasoactive agents. From the second derivative of the plethysmogram, the amplitudes of the second (b) and first (a) inflections are calculated in order to determine their ratio |b/a|. This ratio has been shown to be related to arterial distensibility and severity of atherosclerosis. An advantage of the method is that the finger pulse can be obtained easily, thus making this device useful for epidemiological applications. A comparable device has been developed, on the basis of finger photoplethysmography, and validated in different settings and diseases.”
“Over the past 10 years, a large body of evidence has been collected on large artery stiffening and the wave reflection phenomenon, which have been identified as being the most important pathophysiological determinants of isolated systolic hypertension and pulse pressure increases. Measuring arterial stiffness via changes in vessel diameter in relation to blood pressure changes is complex and not suitable for standard clinical use. On the other hand, measurement of pulse wave velocity provides a comprehensive non-invasive assessment of arterial stiffness, which is simple and accurate enough to be considered as a diagnostic procedure. This is because this measure has been shown to have an independent predictive value for all cause mortality and cardiovascular morbidity, coronary events and strokes in patients with uncomplicated essential hypertension.”
Measurement of Stiffness Index by Digital Volume Pulse Analysis Technique: Clinical Utility in Cardiovascular Disease Risk Stratification by Ashan Gunarathne, Jeetesh V. Patel, Elizabeth A. Hughes and Gregory Y.H. Lip, of the University Department of Medicine, City Hospital, Birmingham, UK.
“Cardiovascular disease (CVD) is the commonest cause of morbidity and premature mortality in the Western world and has rapidly become an epidemic in the developing world over recent years. Given the considerable health care burden conferred by this disease, the timely identification of individuals with an increased risk of CVD is an important consideration.
“The assessment of CVD risk among individuals is usually performed by calculating “risk scores”, such as the Framingham risk prediction score and, more recently, European Society of Cardiology (ESC) HeartScore. Risk score estimation uses a combination of “established risk factors” including age, gender, systolic blood pressure, total cholesterol, and glycemic status. However, these scores are known to underestimate actual risk within high-risk populations, which has led to the quest for novel risk markers for finer and earlier risk stratification.”
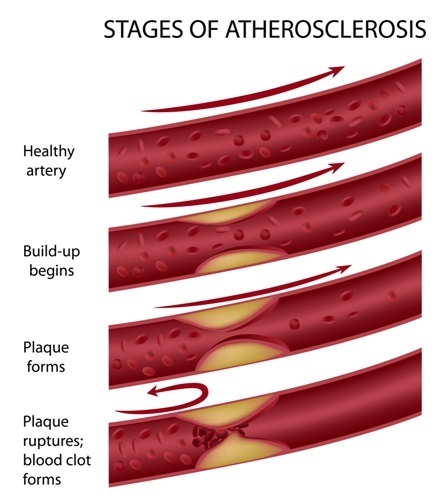
“Central to our current pathophysiological understanding of CVD is closely allied with accelerated atherosclerosis and age-related arteriosclerosis, which are known to alter vessel wall characteristics and increase arterial stiffness. Measures of arterial stiffness indices are accepted as independent markers of CVD having both prognostic and diagnostic implications. The majority of available methods for measuring arterial stiffness have proven to be both technically difficult to perform and time consuming, specifically in terms of their use in risk assessment among large populations and in community settings.”
“In this study, we demonstrate the clinical utility of a marker of arterial stiffness to stratify CVD risk in individuals using the digital pulse wave form analysis technique. This study demonstrates a close association between SI [stiffness index ] and CVD risk score estimation using the ESC HeartScore model. More importantly, the discriminatory properties of the SI in identifying higher risk groups were significantly better than those of conventional cardiovascular risk indices such as total cholesterol level and fasting blood sugar measurements.”
“In conclusion, SIs measured using the DVP [Digital Volume Pulse Analysis] technique is strongly associated with the ESC “HeartScore” cardiovascular risk score and demonstrates the discriminatory utility of the SI in identifying high-risk populations. Thus, noninvasive measurement of arterial stiffness may aid the identification of individuals with high cardiovascular risk.”
IT STARTS IN THE WALL. Early Detection of Vascular Disease through Arterial Waveform Analysis, by Jay N. Cohn, M.D. Professor of Medicine University of Minnesota Medical School Cardiovascular Division

“An advanced technology, Arterial Waveform Analysis, developed at the University of Minnesota, holds the promise of detecting vascular disease at the earliest stages, when subtle changes in the arterial wall provide what appears to be an early marker for vascular disease. Arterial waveform analysis has the potential to assist physicians in positively identifying individuals who exhibit the development of vascular disease and begin appropriate treatment – long before symptoms or clinical signs appear. Arterial waveform analysis may also help physicians improve management of the pharmacological therapy for their patients and aid in efforts to better utilize healthcare resources by allowing therapy to begin much earlier in the disease process, when lifestyle changes and/or lower cost treatments are most beneficial.”
Repeatability of Central and Peripheral Pulse Wave Velocity Measures: The Atherosclerosis Risk in Communities (ARIC) Study by Michelle L. Meyer, Hirofumi Tanaka, Priya Palta, Mehul D. Patel, Ricky Camplain, David Couper, Susan Cheng, Ada Al Qunaibet, Anna K. Poon, Gerardo Heiss, published in the American Journal of Hypertension, Volume 29, Issue 4, 1 April 2016,
“Repeatability was acceptable for all PWV measures in a multicenter, population-based study of older adults and supports its use in epidemiologic studies. Quantifying PWV measurement variation is critical for applications to risk assessment and stratification and eventual translation to clinical practice.”
“PWV is a widely used measure of arterial stiffness and has implications for clinical research and risk stratification. Repeatability was acceptable for all PWV measures in a multicenter, population-based study of older adults and supports its use in epidemiologic studies.”
Digital Photoplethysmography for Assessment of Arterial Stiffness: Repeatability and Comparison with Applanation Tonometry, by Emma von Wowern, Gerd Östling, Peter M. Nilsson, Per Olofsson – 2015
“We performed multiple statistical analyses including numerous PW variables, exposing the study to a risk of a type I error, but we consider that risk insignificant because the study showed consistent and no conflicting results.”
“Arterial stiffness parameters can be determined by applanation tonometry methods, where pressure sensors are placed on superficial arteries, e.g. the carotid, radial and femoral arteries. The carotid-to-femoral PWV is regarded the gold standard to assess arterial stiffness. Although pressure PW analysis shows benefits in predicting cardiovascular morbidity, the impact in clinical practice is small because the tonometry method is cumbersome with a need for highly specialized operators. As an alternative, digital volume PW analysis (DPA) with photoelectric plethysmography (PPG) has been introduced. This technology is inexpensive, easy to use and not operator dependent, which makes it accessible and suitable for clinical practice.” “Although no DPA variable is a surrogate for applanation tonometry variables AIX and PWV, our validation of the DPA against the gold standard method suggests that DPA is a valuable tool for estimation of vascular status. Since the DPA method is fast, relatively inexpensive and operator independent, it could implicate advantages in clinical practice and screening.”
Assessment of Vascular Aging and Atherosclerosis in Hypertensive Subjects: Second Derivative of Photoplethysmogram Versus Pulse Wave Velocity by Luiz A. Bortolotto, Jacques Blacher, Takeshi Kondo, Kenji Takazawa, and Michel E. Safar, from the Department of Internal Medicine, Broussais Hospital, Paris, France
“The pulse wave velocity (PWV) and the photoplethysmogram (PTG) are noninvasive methods for evaluating the pulse wave. The PWV has been associated with age and arterial hypertension, and an index of the second derivative of PTG (SDPTG) is correlated with age and other risk factors for atherosclerosis. The aim of this study was to compare SDPTG and PWV concerning the influencing factors of vascular compliance, including age and atherosclerosis, in a large hypertensive population. We studied consecutively 524 essential hypertensives, 140 with atherosclerotic alterations (AA), defined on the basis of clinical events including coronary heart disease, peripheral vascular disease, stroke, and abdominal aorta aneurysm.”
“The salient findings of this study were that, in a population of treated or untreated subjects with essential hypertension, aortic PWV was strongly related to age, blood pressure, and atherosclerosis.”
“Indeed, in our study, it was possible to perform PWV measurements in a large population of hypertensive patients, providing accurate information concerning modifications in the arterial stiffness related to age or atherosclerosis.”
“…in a large cohort population of hypertensive patients, the PWV was better correlated with the factors that usually induce modifications in the aortic stiffness.”
“In conclusion, the present study has shown, in a cohort of untreated and treated hypertensive subjects, that aortic PWV was a better marker of the presence of AA [atherosclerotic alterations]… PWV seems to be useful for screening of arteriosclerotic independent of age.”
Optical Techniques in the Assessment of Peripheral Arterial Disease by Mohamad E. Alnaeb, Nasser Alobaid, Alexander M. Seifalian, Dimitri P. Mikhailidis and George Hamilton, Vascular unit, Royal Free Hampstead NHS Trust Hospital, London, UK, Academic Division of Surgical and Interventional Sciences, University College London, London, UK, and Department of Clinical Biochemistry and Department of Surgery, Royal Free Hospital and University College Medical School, London, UK
“The fundamental of this technology is the detection of the dynamic cardiovascular pulse-wave, generated by the heart, as it travels throughout the body. The cardiovascular pulse wave is propagated by the elastic nature of the peripheral arteries, as they are excited by the contractions of the heart. The heart instigates a pulse pressure wave that travels throughout the arteries into deeper vasculature. Generally, the illuminating PPG [photo plethysmography] wavelength is chosen to provide weak absorption in tissue, yet stronger absorption by blood, to provide a high degree of optical contrast.”
“Non-invasive optical techniques have become a common method of assessing peripheral vascular function because there is no risk for the patient, and less expense in comparison with duplex scanning. PPG occupies a unique position among these methods. PPG has found considerable use in the field of non-invasive physiological monitoring and the most successful application of PPG in this century is pulse oximetry. Ultimately, the low-cost and simplicity of this optical-based technology could offer significant benefits to healthcare (e.g. in primary care where non-invasive, accurate and simple-to-use diagnostic techniques are desirable). The further development of PPG together with its non-invasive nature can place this methodology among other tools used in the management of vascular disease.”
Waveform Analysis of Peripheral Pulse Wave Detected in the Fingertip with Photoplethysmograph by Irina Hlimonenko, Kalju Meigas, Rein Vahisalu
“Several studies conducted with various groups of population showed significant correlations or powerful interactions between PWV (and other parameters concerning arterial wall circumstances) and the so-called “major” cardiovascular risk factors, such as hypertension, high cholesterol level, diabetes and smoking. Impaired vascular compliance and a concurrent rise in vascular rigidity are the central pathogenetic processes and the first step leading to fatal cardiovascular events in many cases of hypertension and hyperlipidaemia patients. Several methods can be used to analyze the structure and function of the large arteries. Among the noninvasive methods of evaluating arteries, pulse wave analysis can be used as an index of arterial elasticity and stiffness.”
“We suggest that this type of analysis can provide a simple, inexpensive and noninvasive means for studying changes in the elastic properties of the vascular system with the age and disease.”
Correlation between Wave Components of the Second Derivative of Plethysmogram and Arterial Distensibility, by Issei Imanaga, MD, Hiroshi Hara, MD, Samonn Koyanagi, MD, and Kohtaro Tanaka, MD
“The ratio of two wave components b/a constituting the second derivative of the plethysmogram (SDPTG) was correlated with arterial distensibility. Eighty-two subjects (33-93 years old) were classified into three groups according to the thickness of the intima-media complex of the common carotid artery measured by B-mode ultrasonography.”
“These results suggest that a decrease in b/a or in D was proportional to the thickness of the intima-media complex of the carotid artery, that is, the development of atherosclerosis. These results provide direct evidence that b/a of the SDPTG is related to the distensibility of the peripheral artery, and suggest that b/a is a useful non-invasive index of atherosclerosis and altered arterial distensibility.”
“The second derivative wave of the plethysmogram (PTG), the SDPTG, can notably expose the inflection points of the original PTG wave which contains information related to hemodynamics and organic or functional characteristics of peripheral arteries. Therefore, the amplitude and contour of components a, b, c, d, and e constituting the SDPTG have been analyzed in relation to hemodynamics, including cardiac and peripheral circulatory functions and the SDPTG has been evaluated as a useful non-invasive clinical method.”
Assessment of Vasoactive Agents and Vascular Aging by the Second Derivative of Photoplethysmogram Waveform by Kenji Takazawa, Nobuhiro Tanaka, Masami Fujita, Osamu Matsuoka, Tokuyu Saiki, Masaru Aikawa, Sinobu Tamura, Chiharu Ibukiyama
Noninvasive pulse wave analysis is useful for evaluation of vascular load and vascular aging. It is usually measured at the palpable artery, including carotid, femoral and radial arteries. These pulse wave tracings provide more precise information concerning blood pressure changes than systolic and diastolic pressures only. The basic idea of the augmentation index was first described by Murgo et al in 1980 in relation to the reflection return point in the ascending aorta. Kelly et al first used the term “augmentation index” in their 1989 study evaluating age-related changes in AIs. They showed age-related increase in AIs at carotid and radial arteries. Ascending aortic pressure can be divided into 2 components at the anacrotic notch, where maximal flow velocity is observed. The early systolic component is caused mainly by left ventricular ejection, and the second component is augmented by peripheral reflection wave. PTG detects the changes in the amount of light absorbed by hemoglobin, which reflects changes in blood volume.”
“PTG has been used to evaluate arterial compliance in relation to changes in the amplitude of wave, but the wave contour itself is not usually used. The SDPTG [Second Derivative Plethysmograph] has been developed to allow more accurate recognition of the inflection points on the original plethysmographic wave, ie, anacrotic or dicrotic notches.”
Utility of Second Derivative of the Finger Photoplethysmogram for the Estimation of the Risk of Coronary Heart Diseasein the General Population, by Toshiaki Otsuka, MD; Tomoyuki Kawada, MD; Masao Katsumata, PhD; Chikao Ibuki, MD
“We conducted a cross-sectional study in a Japanese community to assess the relationship between the SDPTG indices and coronary risk factors in subjects with no apparent atherosclerotic disorders.”
“In conclusion, the SDPTG indices significantly associated not only with several coronary risk factors, but also with the Framingham risk score in subjects without apparent atherosclerotic disorders at the time of health examination. Furthermore, the b/a screened subjects at risk of CHD with an acceptable sensitivity and specificity. These results suggest that the measurement of SDPTG is useful for the estimation of the risk of CHD in the general population.”
Pulse wave velocity and the second derivative of the finger photoplethysmogram in treated hypertensive patients: their relationship and associating factors,by Junichiro Hashimotoa, Kenichi Chonana, Yohei Aokia, Takuya Nishimuraa, Takayoshi Ohkubob, Atsushi Hozawab, Michiko Suzukia, Mitsunobu Matsubaraa, Mari Michimataa, Tsutomu Arakia and Yutaka Imai.
“Another non-invasive method of evaluating arterial characteristics utilizes the finger photoplethysmogram (PTG). The PTG expresses blood volume changes in the fingertip as pulse waves, but the PTG itself is used only rarely in clinical fields. Instead, the second derivative of the PTG (SDPTG) has been developed for more accurate recognition of the inflection points of PTG. The SDPTG is a simple, convenient and non-invasive technique for pulse wave analysis, seemingly providing information about both central and peripheral arterial factors. In fact, there is a constant relationship between an index derived from SDPTG and the ascending aortic augmentation.”
Complete Articles
Below are a series of full articles. At the bottom of each page are up and down arrows that will take you through each page of the one article.
12-Plethysmograph and Blood Supply 11-Digital_Volume_Pulse_Analysis 10-Arterial_Distensibility 09-Optical_Techiques 07-Photoplethysmogram-2006 06-Finger_Volume_Assessment 04-Pulse_wave_velocity 03-AssesmentOfVascularAging 02-Assessment_of_Vasocative_Agents 01-Dicrotic_Notch_Detection
Science behind the HRV Bar Graphs
Most of the information for understanding the HRV bar graphs is contained in the video above and also in the booklet that comes with the machine. To get an understanding of the scientific support the HRV please contact us- there are hundreds if not thousands of studies on HRV and we can likely find one to answer your exact question. However this article gives a lot of important information and definitions- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5624990. As noted here HRV results are calculated using Time Domain and then separately calculated using Frequency Domain. These are different mathematical approaches to the same data set (the heart beats). Frequency domain gives scores for Total Power, Low Frequency, High Frequency and Very High Frequency and those graphs are shown on our report and also used in some of the other bar graphs. Time domain gives scores such as SDNN and SDRR and many others. These scores are not output. Rather they are used in calculations to create indexes which generate some of the bar graphs on the report.
Here are some of the bar graphs on the Cardio Wave Analyzer report and what they are taken from:
The ANS activity number the TP (or Total Power) which is taken from VLF, LF and HF. Total Power is a common HRV score that is often displayed.
Fatigue number is equivalent to the LF number (low frequency)
Phyical Stress Index is calculated from HR, SDNN & RMSSD
Mental Stress Index Number which is calculated from the LF/HF ratio
Stress resilience index – taken from SDNN.
